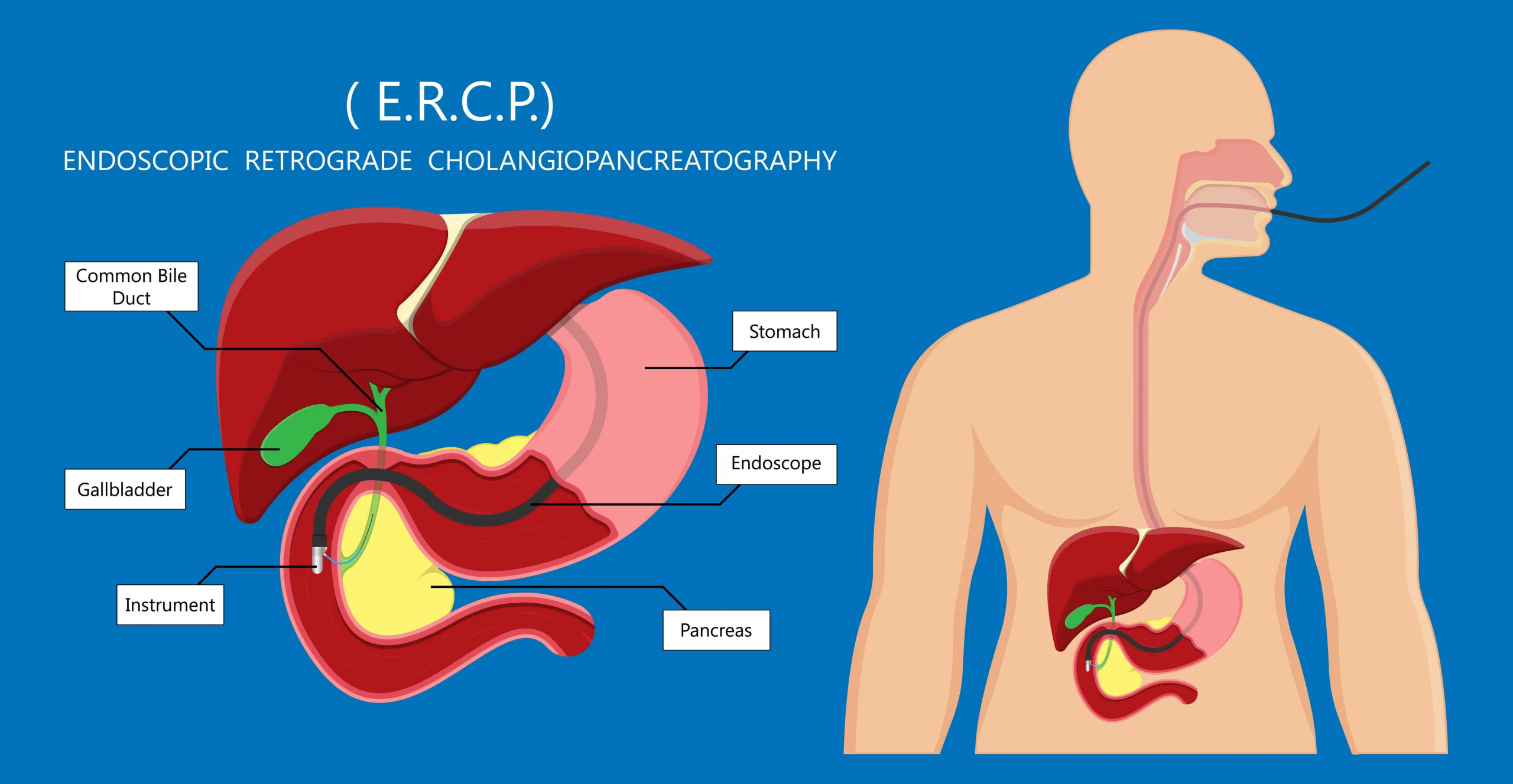
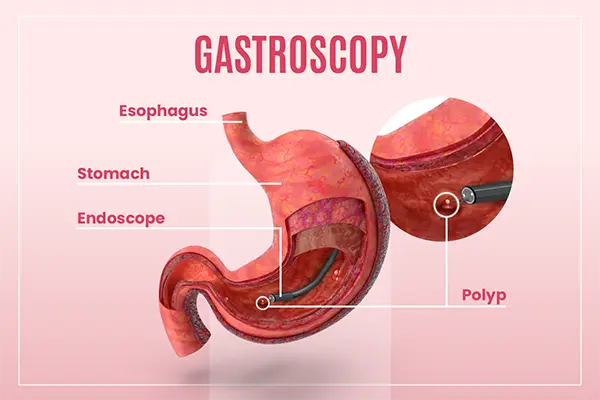
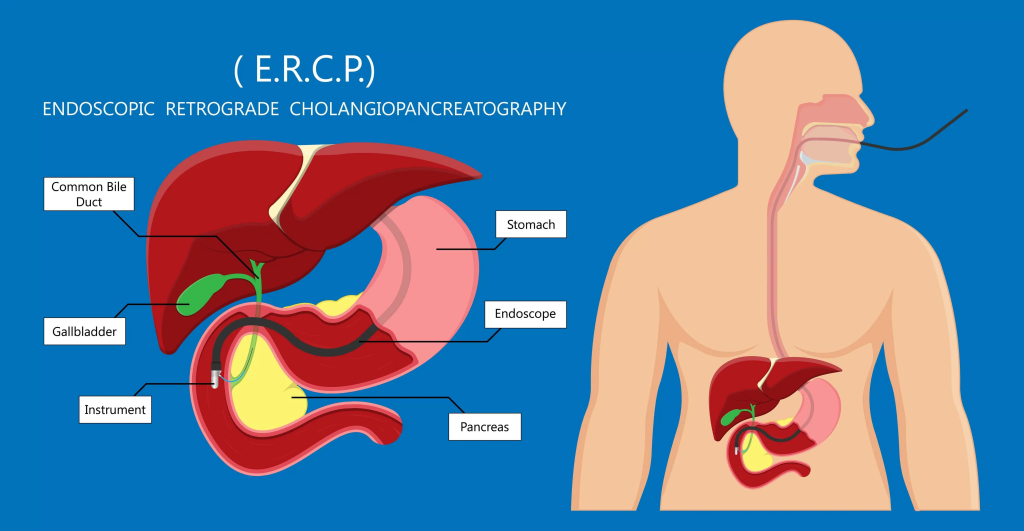
Endoscopic Retrograde Cholangiopancreatography (ERCP) is an advanced therapeutic endoscopy used for bile duct stones, biliary obstruction, and pancreatic disease. Unlike routine gastroscopy, ERCP is technically demanding, with outcomes depending on accurate cannulation, papilla identification, and therapeutic maneuvers.
Key Challenges
- Bile duct cannulation: Failures often result from poor papilla exposure or incorrect scope angle, with risks of post-ERCP pancreatitis.
- Papilla identification: Anatomical variation can hide or displace the papilla, prolonging procedures and raising complication risks.
- Complex anatomy: Duodenal bends and fluid retention obscure visualization and complicate scope control.
- Therapeutic difficulty: Stone extraction, stricture dilation, and stent placement require precision and coordination, especially in complex cases.
Training Strategies
- Optimize patient positioning (prone or semi-prone) to improve exposure and fluid drainage.
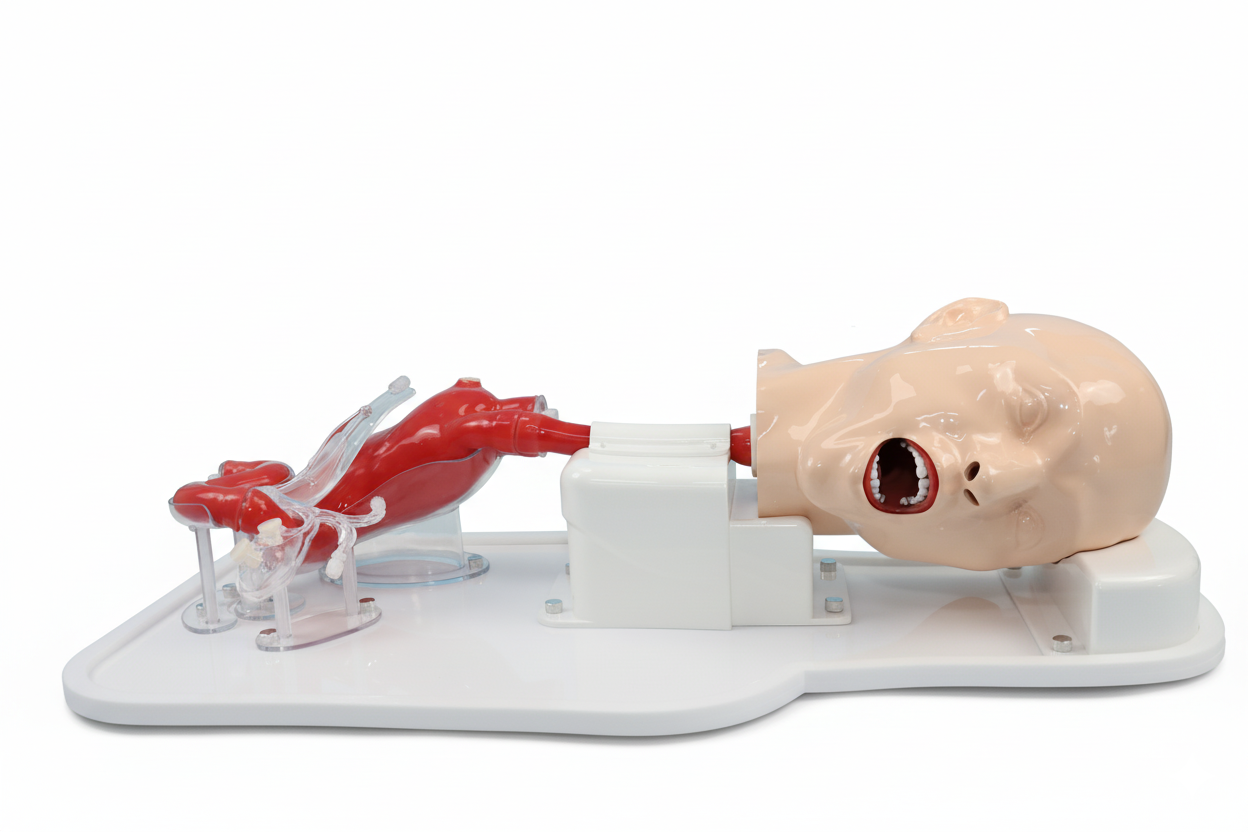
- Use high-fidelity ERCP simulators to practice cannulation, stent placement, and stone retrieval safely.
- Adopt a stepwise curriculum: basic gastroscopy first, then ERCP-specific tasks under simulation.
- Incorporate imaging feedback during practice to strengthen spatial understanding and accuracy.
Key Challenges
- Safe skill development without patient risk.
- Repetition for mastering difficult maneuvers.
- Shortened learning curve from gastroscopy to ERCP.
- Greater confidence and higher clinical success rates.
ERCP is among the most challenging endoscopic procedures. Simulation-based training offers a safe, repeatable, and effective pathway to mastering cannulation, papilla access, and therapeutic techniques—ultimately improving patient outcomes and operator confidence.